Category Sleep Articles
In these articles, I discuss my own experience of sleep problems and sleep topics I find interesting. I also share my tips for sleeping better, and ideas for coping with sleep disruptors, such as noise, light, or heat.


How I Slept After Quitting Caffeine
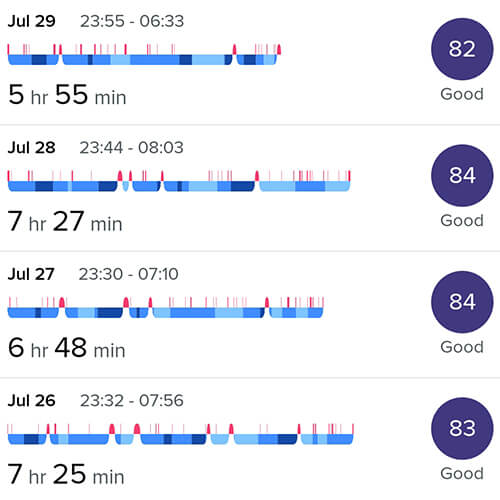
How I Slept During 4 Months Without Alcohol Or Sugar

How Quitting Alcohol And Sugar Affected My Sleep And Health

10 Ways To Keep Your Bed Warm In Winter

10 Things I Do To Sleep Better
Mindfulness Techniques And Resources For Sleep

15 Tips For Keeping Cool In Bed
My Top 12 Tips To Block Out Noise In Bed

I Tested 12 Sleep Teas: These are My Favourites
What Is White Noise And Can It Help You Sleep?

The Best Music For Sleep (With Playlists)
Relaxation Techniques For Sleep

A Bedtime Routine For Adults: 10 Calming Activities